First off I would like to apologize to my subscribers for my 6 week hiatus. On March the 26th, I found out from my children aged 8 and 11 that my ex wife had injected them with the Covid mRNA experiment. Despite being a a registered nurse, and herself suffering side effects from the shot, she forced our kids, who knew that their father was against the “vaccine”, to take it. The worst outcome of a divorce that started shortly after I told my wife I lost my job after saving 3 lives in Rimbey Alberta came true.
My children are not the only ones who have suffered at the hands of people committing injustice in the name of covid. My journey defending the principles of medicine has brought me into contact with many women and men who have endured unconscionable acts. The case of one family who lost their 47 year old father is my substack today. He died not from a viral pneumonia, but from the intentional actions of doctors at the University of Alberta Hospital in Edmonton. His last words spoken over a cell phone to his wife were, “They are putting me under.”
In my entire career as an emergency doctor, the number of times I have put an ER patient able to speak full sentences on a ventilator is 0. If someone is able to call their wife, speak a full sentence in the correct context of a situation without confusion, there is no medical reason they would need emergency ventilation from a machine.
So why did the ER doctor put this previously healthy 47 year old father on a ventilator? Why did he die 5 days later?
What can we find out from his medical record?
Lets look at what the ER doctor Craig Randall Domke wrote:
0152: 47- year old male brought in by ambulance. He is on day 11 of COVID-19 infection. He had worsening dyspnea over the past 4 days. He was seen in Bonnieville where he was hypoxic to 86%. He was given ceftriaxone, azithromycin, dexamethasone, and transferred to Univeristy Hospital for further assessment. His troponin and whole blood D-dimer were negative. During transport he became hypoxic on a nonrebreather at 15L and was subsequently proned for air transport. He is on vaccinated. (perhaps a typo or mis transcribed dictation?)
BP 131/77
Pulse 67
Resp Rate 20
Temp 36.4
SpO2 93%
On examination:
Afebrile, Vital Signs Stable. NAD. Pt Well Appearing.
Neurological: PERRLA, Strong x 4. ALO x 3.
CVS N S1S2, No S3S4, No murmurs. PPP x 4. Warm and well perfused.
Resp: Air entry equal bilaterally, scattered crackles.
GI: Abdomen soft, non tender
Impression plan: 47-year-old male with type I respiratory failure secondary to COVID-19 pneumonia.
Plan: high flow nasal cannula. Dexamethasone as per recovery trial. Tocilizumab. Depsite high flow nasal cannula at 100% the patient desaturated to the mid 80's. The decision was made to pursue rapid sequence intubation. Timeout was made for a compassionate phone call to his wife and children. Following that he underwent rapid sequence intubation with ketamine, fentanyl, and rocuronium. First pass success with video laryngoscopy and a grade 1 view. ARDS-NET ventilatory settings post. Radial arterial line. Admission to ICU.
(Signed)
Craig Randall Domke
0157 6/11/21
Craig Randall Domke
6/11/21 0238
By November 2021, it was well known that mechanical ventilation had high mortality rates. The data from 2020 was over a year old, and dozens of studies were published on the topic indicating that ventilators had high mortality with COVID pneumonia. So from a doctor’s perspective, it would make sense to avoid ventilators and only use them when absolutely necessary, right?
Does a “Vital Signs Stable”, a normal blood pressure, a normal pulse and an oxygen saturation of 93% sound like it needs emergency life support?
Does “NAD. (No Acute Distress) Pt. Well Appearing. ALO x 3. (Alert and Oriented to time, place and person)” sound like someone who needs a ventilator?
Does “Neurological: PERRLA, (Pupils Equal Reactive to Light and Accomodation) Strong x 4. (Four stong and mobile limbs)”, and “Air entry equal bilaterally, scattered crackles.” sound like someone suffering from “Type 1 Respiratory Failure”?
What is Type 1 Respiratory Failure? It is a failure of lungs to take in enough Oxygen to sustain normal life activities like moving and thinking. Does Alert and Oriented and “Strong x 4” limbs sound like a failure of oxygen supply interrupting normal life activities?
Does any of this sound like a respiratory failure? If not, then why is Dr. Craig Domke claiming it is?
(As a side note) type 2 respiratory failure is hypercapnic respiratory failure involving the lungs failing to get rid of CO2. While oxygen levels might be adequate, failure to exhale enough CO2 creates different problems for the body. One common cause of type 2 respiratory failure is giving TOO MUCH oxygen, which fools the brain into thinking it doesn’t need to breathe as often, which leads to an accumulation of CO2 from insufficient ventilation and exhalation.
Dr. Domke’s ER note was signed at 0157, and 0238. It appears that it is very late, and our patient is being treated in the early hours of the morning of November 6, 2021. Maybe the ER doctor was tired and confused. Perhaps he charted the wrong findings or wrote the physical exam from a different patient on our patient’s chart. How do we find out if Dr. Craig Domke’s charting is simply “mistaken”?
Well if other healthcare providers charted similar findings on our patient, then it is unlikely that Dr. Craig Domke’s note was actually a mistake or a mis “recollection” from examining a different patient.
Going against the assertion his charting was “a simple mistake” is Dr. Domke’s statement: "Timeout was made for a compassionate phone call to his wife and children." This part is corroborated by the patient’s wife. Our patient made a cell phone call to his wife, and the last words she heard from him were, “They are putting me under”.
Are there other people on the patient’s medical record who can prove or disprove this ER doctor’s claims? Were there Nurses, Respiratory Therapists, or other doctors?
If so, what did they write? (I’ve abbreviated nurse and respiratory therapist names.)
These notes are from our patient’s chart at the University of Alberta Hospital in Edmonton. It starts with the intake triage nurse’s note on what led our patient to come to Edmonton.
0121 RMM, RN. Sp02 86% on RA, (Room Air) between 2000 and 2150 (in Bonnyville hospital) 02 demand increased from 5L-12L NRB with increased SOB. Bilateral infiltrates on CXR. Arrives on 15L NRB.
0121: Triage electronic: (records from the vital signs machine at triage)
95% on 15L minute.
Temp 35.8
Resp Rate 20. (One breath every 3 seconds)
0150 TW RN. ... Dyspnea for 4 days and increasingly worse, 86% RA, improved to 93% on 15L NRB at 1730. RR: 22-25. No Increase in WOB (work of breathing).
On flight, patient was proned at 15L 95% (Lying face down with a facemask or nasal cannula of oxygen)
So the second registered nurse TW documents oxygen of 93% at 0150 hrs with a respiratory rate of 22-25 with no increase in WOB (work of breathing). Oxygen during the patient’s flight from Bonnyville to the University of Alberta in Edmonton was 95% on 15L of oxygen per minute. At 0121 Hrs upon entry into the ER the oxygen was 95% on 15L oxygen, and the follow up measurements a half hour later were:
0155 ED Vitals
T 36.4
p 67
Sp02 93% (Device Time 0154.35)
BP 131/77 (Device Time 0152.36)
GCS 15
So the oxygen remained 93% at 0154.35 according to the “Device Time”.
So who else observed the Oxygen saturation? Well we have these observations from the respiratory therapist (who manages airway and ventilation equipment for the patient):
0155 ED Vitals:
RT assessment MBO RRT
Temp 36.4
Pulse 67
Resp Rate 20
Sp02 93% (Device Time 0154.35)
BP 131/77 (Device Time 0152.36)
GCS 15
O2 flow 15L/min
THEN A MINUTE LATER!
At 0156 hrs:
RT assessment by MBO RRT
RR 19 (Resp Rate)
SpO2 95% (Device Time 0156.35)
O2 60L min
Why did the respiratory therapist turn the Oxygen up to 60L a minute?
At 15 L/min facemask oxygen, the patient’s oxygen saturations were basically unchanged since the airplane flight where it was 95% during the flight and then 93% at 0155 in the ER. Was there a sudden change in the patient’s status to justify having the oxygen turned up to 60 liters per minute? A 400% increase in oxygen? Was the patient suddenly having trouble breathing?
Well at 0156 hrs, the respiratory therapist MBO did chart an equipment check, and a note that the patient was receiving the 60L of oxygen via heated humidified optiflow nasal cannula, and that the respiratory rate was an unremarkable 19 breaths per minute. (One would think that a the respiratory therapist would not be charting equipment checks if the patient was suddenly deteriorating.)
The full respiratory assessment at 0201 hrs:
RT assessment by MBO RRT
Resp Rate 14
SpO2 93% (Device Time 0159.35)
O2 60L/min
Resp pattern Tachypnea
Resp Depth Shallow
Resp Effort, Unlaboured
Dyspnea Occurrence Not Observed
Chest Inspection Symmetrical
Cough Non-productive, constant spontaneous strong
Resp: 14 (Device Time 0200.35)
Why go into all this excruciating detail? Well if a patient is getting more oxygen than he needs, breathing tends to be shallow. How 14 breaths a minute (about one breath every 4.5 seconds) is charted by MBO as “Resp pattern Tachypnea” (fast breathing) makes no sense. Also notable here is that she charts that the respiratory effort is “Unlaboured”, and that “Dyspnea Occurence” was NOT observed (no observation of dyspnea — the distress from not getting enough air). These observations, however, are consistent with Dr. Craig Domke’s physical examination that provides no evidence of respiratory failure or necessity of a ventilator.
Furthermore, the respiratory therapist MBO charts “Cough Non-productive, constant spontaneous strong”. This also agrees with Dr. Craig Domke’s physical examination. Our patient is not exhausted from hours or days of difficult breathing. He still has a strong spontaneous cough, which is the body’s reaction to clear the lungs. If a cough is constant AND strong, there is no evidence of “Type 1 respiratory failure”. A “respiratory failure” from lack of oxygen usually causes unconsciousness leading to an absence of cough, or lethargy causing a weak cough.
None of the care providers documented any oxygen less than 93% following the patient’s arrival at the University of Alberta Hospital in Edmonton. In fact the respiratory therapist MBO offers no reason for the 400% increase in oxygen from the previous 15L/min that seemed to keep the patient alert and in “No acute distress” both in the ER and for hours prior during his airplane flight.
Too much extra oxygen can cause lung damage. It can also lead to decreased stimulus for respiration that in turn causes excess CO2 in the blood from slower rates of breathing. This problem can be all too familiar to patients who have COPD, where an oxygen saturation in excess of what the body needs, leads to CO2 narcosis, — a case where the patient’s lack of breathing from too much supplemental oxygen, leads to a buildup of CO2 in the blood causing hypercarbia confusion and lethargy. Typically for the COPD patient, oxygen saturations are kept no higher than 88% to prevent this acute side effect of “too much oxygen”. In the ICU, oxygen toxicity causing damage to lung tissue is also a well known problem, and the longer the exposure to excessive concentrations of oxygen, the worse the lung damage. Ventilator protocols developped from decades of studies and reviews of patients with lung injury, reduce oxygen concentrations back to normal room air levels as quickly as possible to prevent lung damage. Aside from situations where higher oxygen saturations may be necessary to prevent further damage in the setting of a heart attack or stroke, supplemental oxygen in awake and alert patients should be kept to a minumum in any competent healthcare facility.
The ER doctor Craig Domke claims his patient needed to be put on a mechanical ventilator for a “Type 1 respiratory failure”, but there is no documented low oxygen, and there are no signs of respiratory failure FROM ANYONE. Dr. Domke’s note has no mention of lethargy or weakness. Notes from 2 nurses and a respiratory therapist have no mention of lethargy or weakness. A patient with unlaboured breathing, who is alert and moving all 4 limbs has enough oxygen for the normal functions of life. How can Dr. Craig Domke claim our patient has a type 1 low oxygen failure of the respiratory system?
Perhaps there was something he saw in the blood tests?
Something so critical that it required emergency life support to prevent death?
Let’s look.
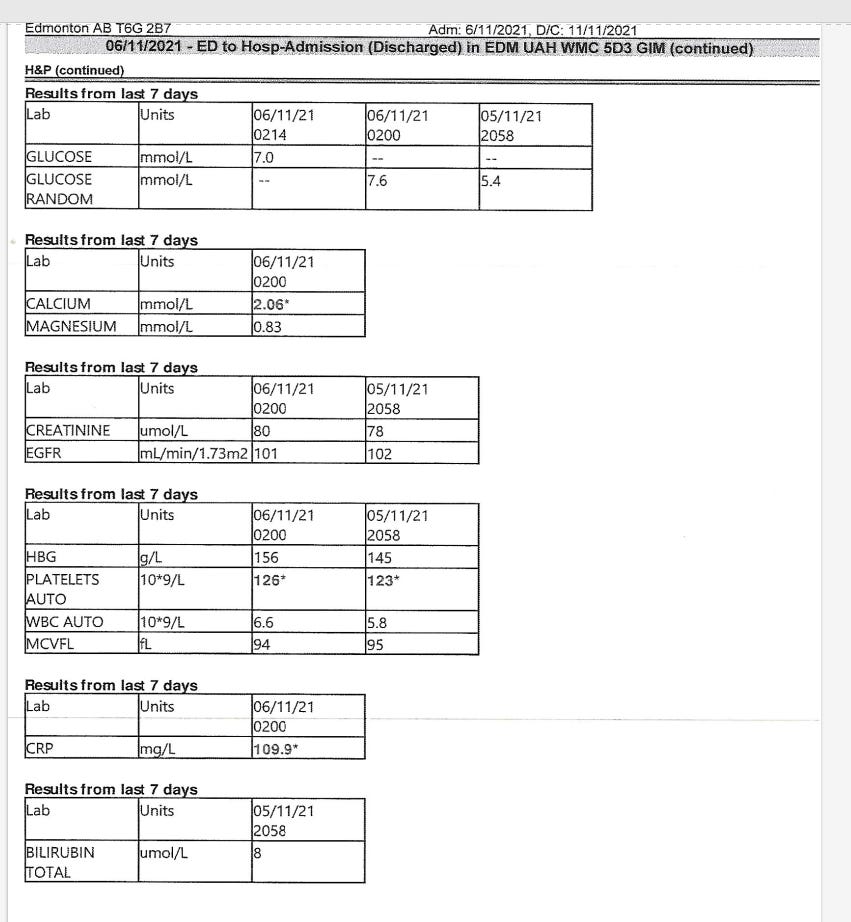
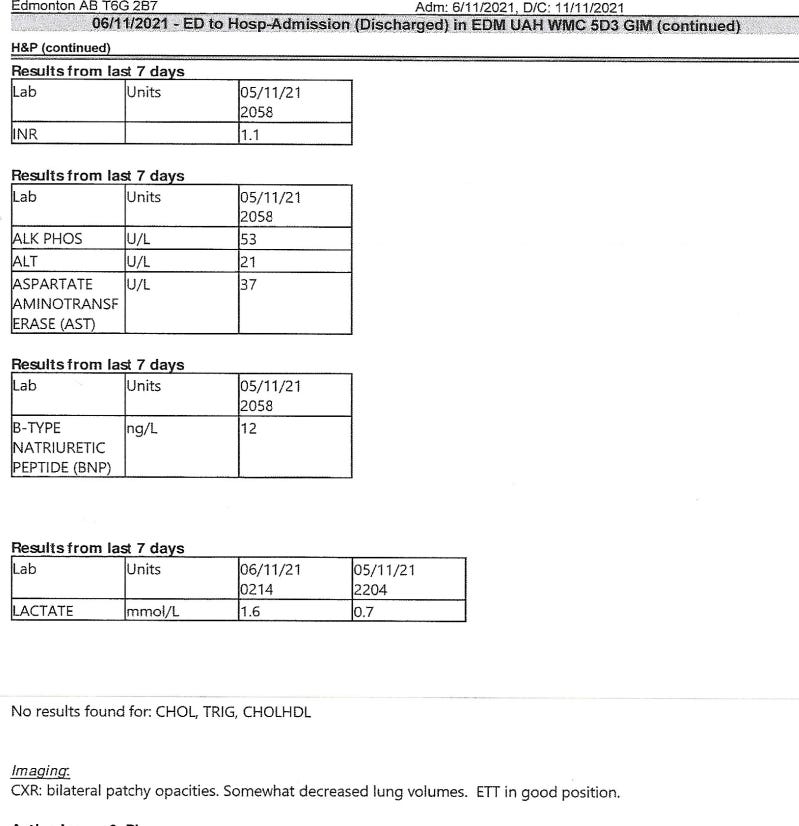
His blood tests from the night before and that morning were all normal except for slightly low platelets of 123 and 126 (from the night before and morning respectively), and a CRP (measuring inflammation) of 109. His lactates were normal, twice indicating he did not have sepsis (blood infection).
What else is there?
Venous Blood Gas 0218:
pH 7.34 (7.3-7.4)
pCO2 51 (35-50)
pO2 27 (30-50)
HCO3 28 (20-27)
BE 2 (-4 - 1)
O2 Sat 43% (50-80)
The venous blood gases results above are normal for a patient undergoing metabolic stress. A body fighting a viral infection is expected to have increased cellular activity and therefore oxygen use. This would be most apparent in the venous blood that is coming out of tissues to return to the heart and lungs. The pO2 (partial pressure of Oxygen) was slightly low at 27 in our patient. The normal ranges from 30-50. 27 represents a deficit of about 10%. This indicates that our patient’s tissues were using more oxygen and producing more CO2 than usual, but far from what we would see in a critical illness. A pCO2 of 51 is just slightly higher than the normal range of 25-50 in venous blood.
11 minutes after a mostly normal venous blood gas, at 0229, our patient is documented as having been intubated, and 2 minutes later documented to be on a ventilator.
Again. Why was the patient put on a ventilator?
The blood tests offer NO explanation.
Did other Doctors concur with Dr. Craig Domke’s deadly decision?
Yes, a Dr. Alistair Eksteen shows up on the chart as an assistant in putting the patient on a ventilator. Then a Dr. Michael Jacka from the ICU is on the record as accepting the patient to the ICU. No protest of the decision to put the patient on life support is documented by Dr. Alistair Eksteen or Dr. Michael Jacka. Nor did either doctor remove the patient from the ventilator later that day, despite the documentation in the consult note signed by the internal medicine Resident Dr. Olivia Friesen at 0622 hrs which stated: "Pt not tolerating vent, taking in varying tidal volumes (either too small or too large) Given Roc which improved vent synchrony."
When a patient is documented “not tolerating the vent”, it is a sign that the patient is awake. During standard ICU assessments to see whether a patient needs a ventilator, a patient who takes in varying sizes of breaths, overriding the breath settings of the machine, is a sign of consciousness, indicating that the patient may be able to breath just fine without a ventilator. “Given Roc which improved vent synchrony.” means the patient was given a paralytic to stop the patient from breathing against the ventilator settings.
Who does that? Paralyses a patient who might be struggling against a ventilator because he is awake?
But it gets worse. If that was not enough, an infectious diseases specialist Brittany Kula MD orders baricitinib, a medication with a black box warning for increasing infections, blood clots and higher rates of mortality. Not only did this medication originally developed for rheumatoid arthritis patients cause cancer, it also increased heart attacks. In short, this medication INCREASES a patient's chances of dying from all causes1.
Dr. Brittany Kula, on a patient who is unable to refuse a dangerous and unproven medication, orders the medication baricitinib that is PROVEN to increase death at 0555 hrs on November 6th, 2021.
He died 5 days after Dr. Brittany Kula’s order. The cause, as verified by autopsy, was from multiple blood clots in the lungs — a side effect so common it is listed as one of the black box warnings for baricitinib.
Did he need this deadly medication? Almost 3 hours after being put on a ventilator, our patient’s oxygen saturation was 98% at 0510.29 hrs and 100% at 0530.00 hrs. From intubation at 0229 hrs, till 0530 hrs there was nothing about the lungs that impaired oxygen delivery to the point of needing a deadly unproven medication. But Dr. Kula ordered baricitinib anyway at 0555 hrs.
Had doctors simply continued antibiotics and dexamethasone (a steroid), and sent our patient to a regular ward his chances at living would have been far better.
So what do all these unexplainable actions by multiple doctors add up to?
If I had pursued a career as a detective, and I found a case where multiple people engaged in multiple actions all directed towards killing someone, I would investigate it as a homicide.
Is the College of Physicians and Surgeons of Alberta investigating Dr. Craig Domke over his patient’s death?
Has the College of Physicians and Surgeons of Alberta investigated Dr. Alistair Eksteen for assisting Dr. Craig Domke in the death of a patient?
Has the College of Physicians and Surgeons of Alberta investigated Dr. Michael Jacka for torture? (Signs that a patient was awake on a ventilator but administering drugs to paralyze the patient?)
Has the College of Physicians and Surgeons of Alberta investigated the infectious diseases specialist Dr. Brittany Kula for ordering a deadly drug?
Not as far as I know.
But I myself have been investigated for saving the lives of 3 patients with Ivermectin. I have had my Emergency Room work ended by Alberta Health Services and the Alberta College. I have had restrictions placed on my license that make it impossible for me to work as a doctor. So what is the point of having a medical college?
Why name all the doctors?
I do so because it is my duty to protect patients.
The College of Physicians and Surgeons of Alberta have failed to protect patients from homicide.
The provincial prosecutor has not investigated Alberta Health Services for homicide.
Politicians certainly are not protecting patients from homicide.
The College of Physicians and Surgeons of Alberta and Alberta Health Services withheld life saving medications from patients.
Remember our patient’s last words.
“They are putting me under.”
The best I can do is warn the public.
Addendum for further Medical interpretation:
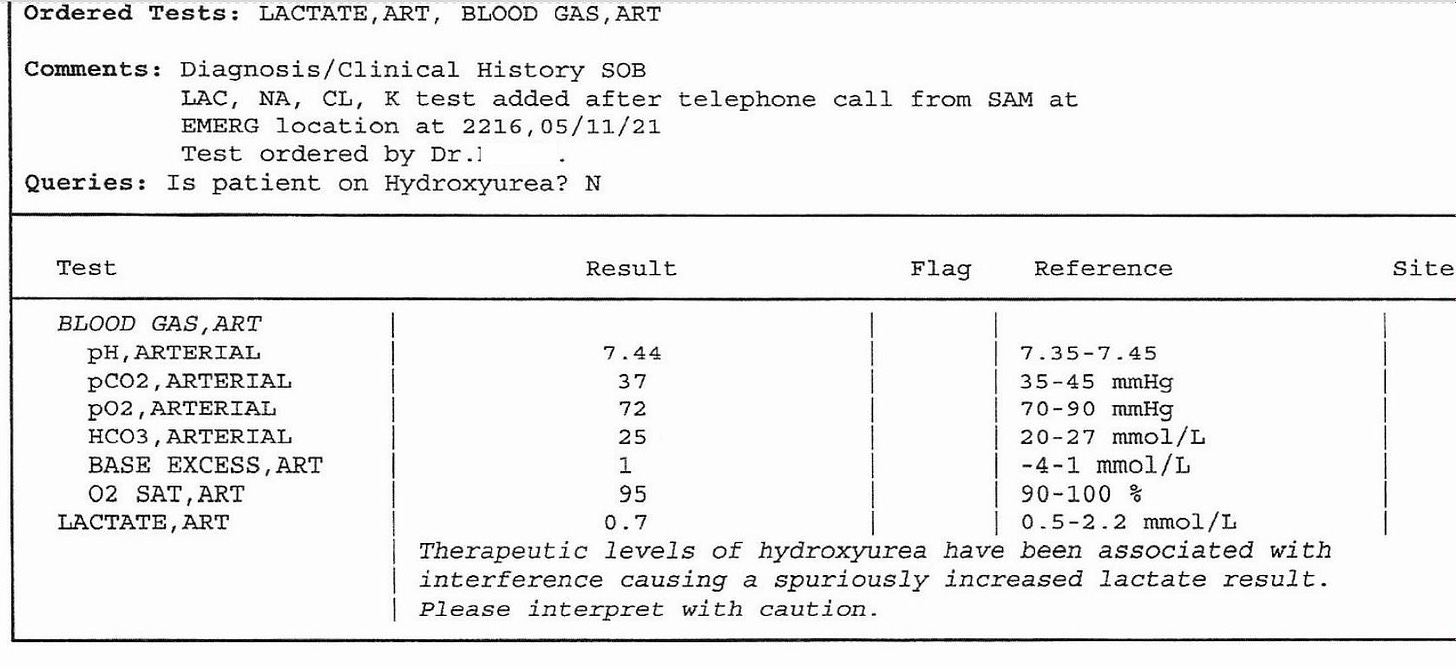
This is the patient’s Arterial blood gas prior to his transfer to from Bonnyville Hospital and University of Alberta in Edmonton:
As an ER doctor, I’d be very happy to see an ABG like this for a patient. It tells me that my patient’s lungs are doing just fine. So why did the Bonnyville doctor transfer our patient?
https://reference.medscape.com/drug/olumiant-baricitinib-1000107#5
*Permission was granted from the widow to publish this case.


Sorry to hear about what happened to your children.
I can only imagine the primal rage a knowing parent must feel about this.
Hopefully, the truth will come out soon. If it does, we'll hopefully have time to rectify a lot of the damage that's being done. (I bet that people will be focused on finding remedies, and since necessity is the mother of invention, there will be little in the way to stop people from doing this.)
Thanks for giving this man's story a voice.
That's an example of speaking for those who don't have a voice.
I am so sorry Dr. Negase, I too am concerned for my kids. They wouldn't listen, plus early on I was still in a fog myself. Prayers and thanks for getting the truth out no matter the consequence. Amy.