The Difference Between Negligence and Homicide
a process of thought
When I testified at Canada’s National Citizen’s Inquiry I spoke about homicide in the hospital. In the 1/2 hour I was scheduled to speak I did not have the time to explain why I chose homicide versus the more common claim of malpractice or negligence.
Here is the National Citizen’s Inquiry Video:
When I read through the charts of patients who died in hospital, I took the approach of questioning, “Was this death preventable?”.
If the death was preventable, what were the mistakes?
However, I quickly realized that what I was reading did not contain mistakes, rather the medical record detailed deliberate actions resulting in the patient’s death.
This forced me to contemplate the difference between negligence and homicide. Specifically, I had to find the dividing line between negligence causing death and homicide.
One of the cases in question, I analyzed in detail in my post:
A deadly day in the ER
First off I would like to apologize to my subscribers for my 6 week hiatus. On March the 26th, I found out from my children aged 8 and 11 that my ex wife had injected them with the Covid mRNA experiment. Despite being a a registered nurse, and herself suffering side effects from the shot, she forced our kids, who knew that their father was against the…
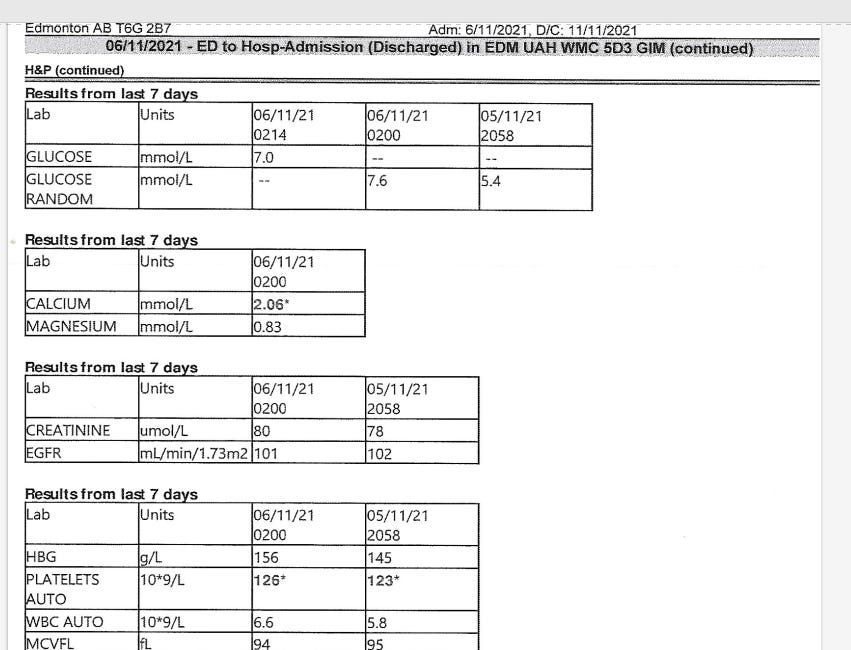
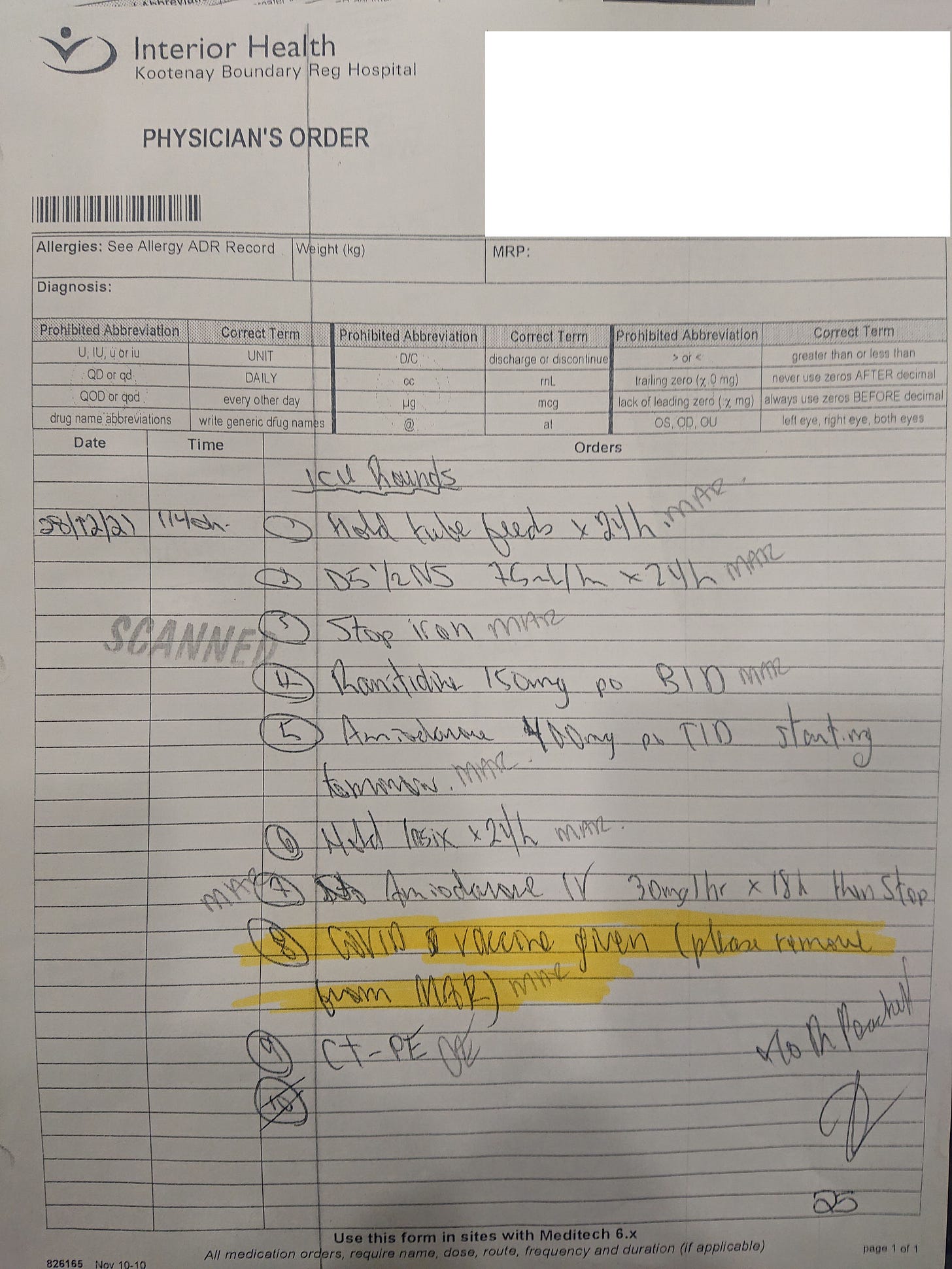
The second case I mentioned in the NCI testimony was a situation where Dr. Peachell, the head of ICU in Trail hospital BC, ordered the Pfizer COVID-19 injection for a 69 year old patient who was still recovering from COVID pneumonia. The week prior she improved enough to no longer need a ventilator. However, 7 days after breathing fully without the assistance of a ventilator, Dr. Peachell ordered the Pfizer mRNA injection on December 24, 2021. 4 days later he gave a verbal order to remove Covid 19 vaccination from the medication administration record (MAR). Clinical deterioration was noted by another ICU physician by the 29th. On the 30th, care was reduced to comfort measures only, and she died shortly thereafter.
Negligence vs. Homicide
To come to terms with these tragedies, I had to first ascertain whether what I had witnesed in the medical records was malpractice, or homicide. Here are the 3 principles I used to differentiate the two.
1) Action vs inaction.
Inaction causing death can be negligence. However, in the case of A Deadly Day in the ER there was action.
If the patient had simply been left alone, with no changes to his previous treatment, he would likely be alive today.
Similarly, if the patient of Dr. Peachell had simply been left alone to complete her recovery from covid pneumonia without being injected with the Pfizer injection, she would likely have continued her recovery.
2) If death was the result of an action, was the action
a) Deliberate
OR
b) Accidental
Since there is no way to "accidentally" put someone on life support or "accidentally" prescribe a black box warning medication like baricitinib, then the actions that resulted in death were deliberate.
3) If there was deliberate action, was that action made with knowledge that the action would cause harm? This one is harder to answer. I can only speak to what is expected from an ER doctor or a Specialist as far as knowledge is concerned.
As of 2021 Mechanical Ventilation was known to be associated with higher mortality. Was Dr. Craig Domke at the University of Alberta ER aware of this?
Baricitinib has a black box warning for deadly side effects. Was Dr. Brittany Kula a specialist at the University of Alberta department of infectious diseases aware of this?
All I can say is they should be aware of the harms associated with any treatment. This is the most basic requirement of doctors.
But suppose both doctors denied knowledge of the harms of their treatments. Would their actions be justifiable in other ways because they were treating an emergency and did not have the time to balance benefits versus harms? e.g. They acted in a panic to an emergency, and did not contemplate or inform their patient of the risks of treatment?
Would a physician as such be competent physician in an ER?
Was there such a time critical emergency in the ER?
The patient arrived in the ER at 0152, and was intubated (put on a mechanical ventilator) at 0229hrs, over a half hour later. In Dr. Craig Domke’s dictation he mentions “Timeout was made for a compassionate phone call to his wife and children.” This I confirmed with the widow.
DOES THIS SOUND LIKE THE TYPE OF EMERGENCY WHERE SPLIT SECOND DECISIONS HAVE TO BE MADE? WHERE SECONDS MATTER?
Ok, maybe it was a slow emergency in progress…(back to the article A deadly day in the ER).
Was the patient suffering from any signs of inadequate oxygen? For example, unconsciousness, lethargy, or weakness?
Was the patient suffering from objective evidence of inadequate oxygen such as a heart attack, kidney failure or stroke?
Any of these factors might provide reason for putting the patient on a ventilator. However, signs of a critical medical emergency were conspicuously absent from the medical record.
For Dr. Craig Domke, an ER doctor, to claim ignorance of the risks of ventilators would make that individual incompetent to be working in a hospital.
To claim he had knowledge of ventilator risks but didn’t have time to reasonably contemplate those risks for an optimal medical decision over 1/2 an hour in the absence of a critical deterioration in the ER… seems untenable.
To hypothetically use ignorance of risks of mechanical ventilation, or a lack of time as a as a mea culpa for his fatal decision would be dishonest.
How about Dr. Brittany Kula and her use of Baricitinib?
Well the Alberta Health Services guideline on COVID says: “Baricitinib is approved for use in patients with severe COVID-19 pneumonia. To be eligible patients must be experiencing significant progressive respiratory failure due to COVID-19 pneumonia that requires they receive ventilation (invasive or non-invasive) or supplemental oxygen to achieve a minimum SpO2 of 90%.1
The one thing that was consistent in our patient’s medical record was how stable his oxygen was at 93% or greater, both prior to and after being put on a mechanical ventilator.
For a specialist to “hypothetically” claim ignorance of a black box warning on a subspecialty medication AND Alberta Health Services own guidelines for use of a new medication would be dishonest.
For an infectious diseases specialist to claim that somehow the patient had “significant progressive respiratory failure” when the chart documents oxygenation of 100% after 3 hours of mechanical ventilation, is untenable. To try and claim use of an experimental black box warning medication WITHOUT the patient’s consent is justified would be dishonest.
So we have made 3 observations:
Doctors at the University of Alberta took:
1) Actions.
These actions were:
2) Deliberate
These deliberate actions were made with:
3) Knowledge of the consequences.
So was this negligence? Death from inaction?
Was this malpractice? Death from accidental actions?
Or was this premeditated homicide? Death from deliberate actions made with knowledge of what consequences those actions would lead to.
You decide.
https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-recommendations.pdf

Doc we got your historical testimony edited and captioned here: https://rumble.com/v2p5kr8-dr.-daniel-nagase-investigating-medical-evil-nci-full-testimony-with-captio.html
Your testimony had, by an order of magnitude, the most attention of ANY tweet we made during the NCI. We can't imagine what you've been through, but we want you to know you're reaching people! Here's the tweet that blew up (excuse the slight inaccuracies with the specifics in the tweet. J from the channel was tweeting live and doing the best he could. We added correction under the tweet): https://twitter.com/super_spreaders/status/1659614268189229066?s=20
I think you did a really great job testifying 💯
Thank you 🙏